When a workplace accident occurs, it can be a stressful and scary situation for both your injured employee and you, the employer. The employee is injured, potentially can’t work, and is worried about how they can pay bills. The employer is worried about losing a valued employee, the impact on co-workers, and the challenge of navigating an unknown workers’ comp process in an effort to get the employee healed and back to work.
Understanding the process can make the situation much easier for both the employee and employer. The primary objective is to get the injured employee healthy and back to work with their peers.
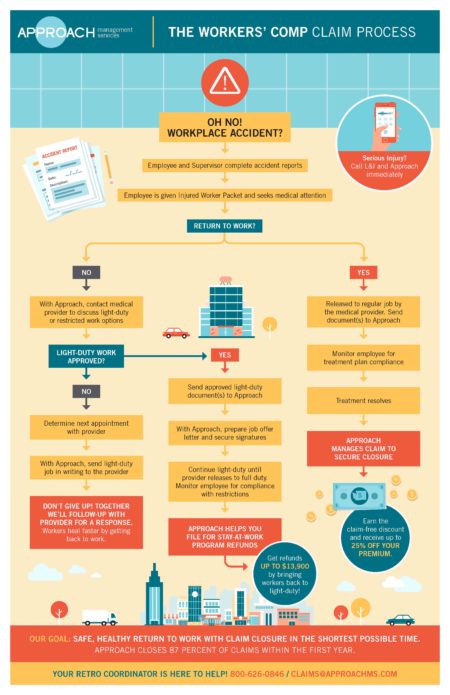
View our flowchart of how the claim process works.
This is ideal for new employees not use to managing workers’ comp claims.
How the claims process works
- When an accident occurs, make sure the employee reports the incident to a designated contact within your organization.
- Have both the employee and the supervisor complete an accident report of what happened.
- If medical attention is required, offer to transport the employee to a medical provider of their choosing. Make sure the employee is given the Injured Employee Packet for completion by themselves and the medical provider.
- If the medical provider issues a treatment plan and releases the employee back to light-duty/restricted work, the employer should monitor the employee to make sure they are in compliance with the treatment plan and work restrictions. For example, if the medical provider dictates that the injured employee can’t lift anything over 25 lbs. for four weeks, under no circumstances can you allow the employee to lift 25 lbs., even if the employee indicates that they “feel better”. You must make sure the medical provider removes the 25 lbs. restriction before the employee can perform that activity again.
- While the employee is following his/her treatment plan, the employer needs to send the accident reports, completed Injured Worker Packets, treatment plan, and any other documentation to your Approach retro coordinator who will assist with ensuring all appropriate measures (and regulatory compliance) have taken place.
In most cases, treatment resolves and the claim closes.
What if the medical provider doesn’t release the injured employee to light-duty or restricted work?
There are many options that can be explored, too many to list. If light-duty or restricted work is not an option provided by the medical provider, we’d strongly advise you to seek the assistance of a third-party administrator such as Approach Management Services. At Approach, we are here to guide you through the claims process. We understand that an early and safe return to work is critical to an injured employee’s recovery. Studies show that injured employees who return to productive work as soon as possible heal faster and better than those who don’t.
Contact your Approach Retro Coordinator for next steps and keep in frequent contact with the medical provider. If you are not a client of Approach Management Services contact us today at 1-800-626-0846 to learn how we can assist you.
REMEMBER – As an Approach client we are here to help you every step of the way and it’s never too early to involve us when an accident occurs.